| Journal of Food Bioactives, ISSN 2637-8752 print, 2637-8779 online |
| Journal website www.isnff-jfb.com |
Review
Volume 22, June 2023, pages 17-26
Therapeutic potential of nutritional food for a healthy cardiometabolic system—a review of molecular mechanism
Ravindra Vermaa, *, Prakash S Bisena, Mònica Bullób, c, d
aSchool of Studies in Biotechnology, Jiwaji University, Gwalior 474011, India
bDepartment of Biochemistry & Biotechnology, University Rovira i Virgili (URV), Spain
cNutrition and Metabolic Health Research Group, Institute of Health Pere Virgili (IISPV), Spain
dCIBER Physiology of Obesity and Nutrition (CIBEROBN), Carlos III Health Institute, Spain
*Corresponding author: Ravindra Verma, School of Studies in Biotechnology, Jiwaji University, Gwalior, 474011, India. Tel: +91-11-7999212685; E-mail: vermaravindra917@gmail.com
DOI: 10.31665/JFB.2023.18345
Received: June 10, 2023
Revised received & accepted: June 23, 2023
| Abstract | ▴Top |
Nutritional therapy and disease causes have been studied sparingly. It is one of the main objectives of this study to look for a nutritional diet that promotes cardiovascular health. Various electronic databases and scientifically published articles were searched for relevant information for this review. In addition to these parameters, diabetes, blood pressure, smoking, lifestyle, and inactivity also play a significant role in these diseases. Various scientific studies have shown that consuming the right kind of food, following healthy eating habits, and leading a healthy lifestyle can reduce the risk of heart disease and stroke. The gut microbiome and cardiovascular risk have been shown to be significantly affected by vegetarian and Mediterranean diets. As an adjunct to traditional drug treatment, a healthy lifestyle and a proper diet are essential to improving cardiac patients’ lipid profiles. It is essential to understand CVD’s molecular and cellular mechanisms and develop targeted therapies.
Keywords: Cardiometabolic; Food; Lipid; Metabolical; Nutrition
| 1. Introduction | ▴Top |
Human health is significantly affected by food and eating habits. People search for healthy foods and supplements online and become obsessed with what they should eat. The importance of eating body-balanced foods is widely acknowledged to be lacking in society. There are differences in the types of foods available in different geographical regions, as well as the types of eating habits (Gao et al., 2021). According to WHO (2021), 17.9 million people died from cardiovascular disease in 2019, which was equivalent to 32% of all global deaths in 2019. As Stoney et al. (2018) have noted, cardiovascular disease has been the leading cause of death worldwide for the past 50 years. A healthy diet, exercising more, quitting smoking, and controlling obesity can all help prevent this unusual death rate. It was found that fast food consumption is strongly associated with sleep disturbances caused by stress (Khan et al., 2021). As mentioned above, cardiovascular disorders are associated with unhealthy eating habits. It is also controversial how food habits affect the risk of heart attacks. Numerous studies have shown that high fat intake does not have a meaningful effect on heart attacks or cardiovascular disease (Dehghan et al., 2018). “Is there more to a healthy-heart diet than cholesterol?” by science columnist Healey claims that high saturated fat in the diet can reduce strokes by 20% (Healey, 2021). A variety of compounds are found in food, but most people are unaware of their nutritional importance. Milanlouei et al., (2020) identify 16 foods and 37 nutrients that are significantly associated with coronary heart disease risk is revealed in a systematic review of 257 nutrients and 117 foods with coronary heart disease risk (acute myocardial infarction and fatal coronary heart disease). There is strong evidence to suggest that eating fruit and vegetables on a regular basis can significantly reduce the risk of coronary heart disease and heart failure (Pallazola, et al., 2019). This article provides a brief review of current research in the field of food and metabolic disorders, including those associated with cardiovascular disease. A healthy diet is essential to maintaining a healthy heart, so the purpose of this article is to provide information about doing so. The relationship between diet quality, quantity, and cardiovascular health is crucial for understanding the body’s requirements and eating habits (Millar et al., 2021). The term cardiovascular health (CVH) refers to a combination of health indicators and habits such as body mass index (BMI), a healthy diet, physical activity, smoking status, blood pressure, glucose, and cholesterol levels. People with poor CVH have a higher risk of cardiovascular disease (Gaye et al., 2020). As a result of elevated self-efficacy and a decrease in stress, young adults may eat less sugar and consume a diet of lower quality, which will lead to improved eating habits (Francis et al., 2019). Nature offers a wide variety of dietary options that can benefit our health and cure metabolic-related disorders. The father of modern medicine Hippocrates said, “Food is medicine and medicine is food”.
| 2. Material and methods | ▴Top |
In order to perform this study, a systematic electronic database search as well as a review of scientifically published articles relevant to the topic was conducted. An analysis of five years’ worth of articles (2018–2023) was conducted. Various scientific databases use Boolean search methods, including Google Scholar, PubMed, and Mendeley, etc. Search engines use terms like food for a healthy cardiovascular system, metabolic disorders, Type-2-Diabetes (T2D), food and/or metabolic disorders, food and/or T2D, food and/or cardiometabolic disorders, etc.
| 3. Result and discussion | ▴Top |
3.1. Causes of cardiovascular disorders
Modern medicine does not offer a viable solution to metabolic-oriented diseases like cardiovascular disease and diabetes (Bodai et al., 2018; Reddy et al., 2019). Several studies have shown that nutritional therapy in conjunction with a healthy lifestyle can lead to an early recovery in metabolic diseases (Kadhim and Mohammed, 2021; Mahboub et al., 2021). The right combination of dietary choices can enhance our health and treat metabolic disorders (Figure 1). It has been shown that consuming a large amount of fruits and vegetables reduces the risk of cancer and cardiovascular disease (CVD) (Liu et al., 2021). It has been observed that heart failure and atrial fibrillation rates are increasing among healthy individuals, but the reasons for this are unknown (Guasch et al., 2018). A wide variety of cardiovascular diseases are associated with acute care for hemodynamically unstable patients, interventions for coronary obstructions and disorders associated with electrically wobbly rhythms, as well as disease prevention and treatment. Various lipid oriented cardiometabolic disorders are mentioned in Table 1. The risk of heart disease is increased by high blood pressure, high cholesterol, and smoking. Diabetes, overweight and obesity, poor diet, lack of exercise, and excessive alcohol consumption are also factors that contribute to heart disease (Zhang et al., 2019: Piché et al., 2020).
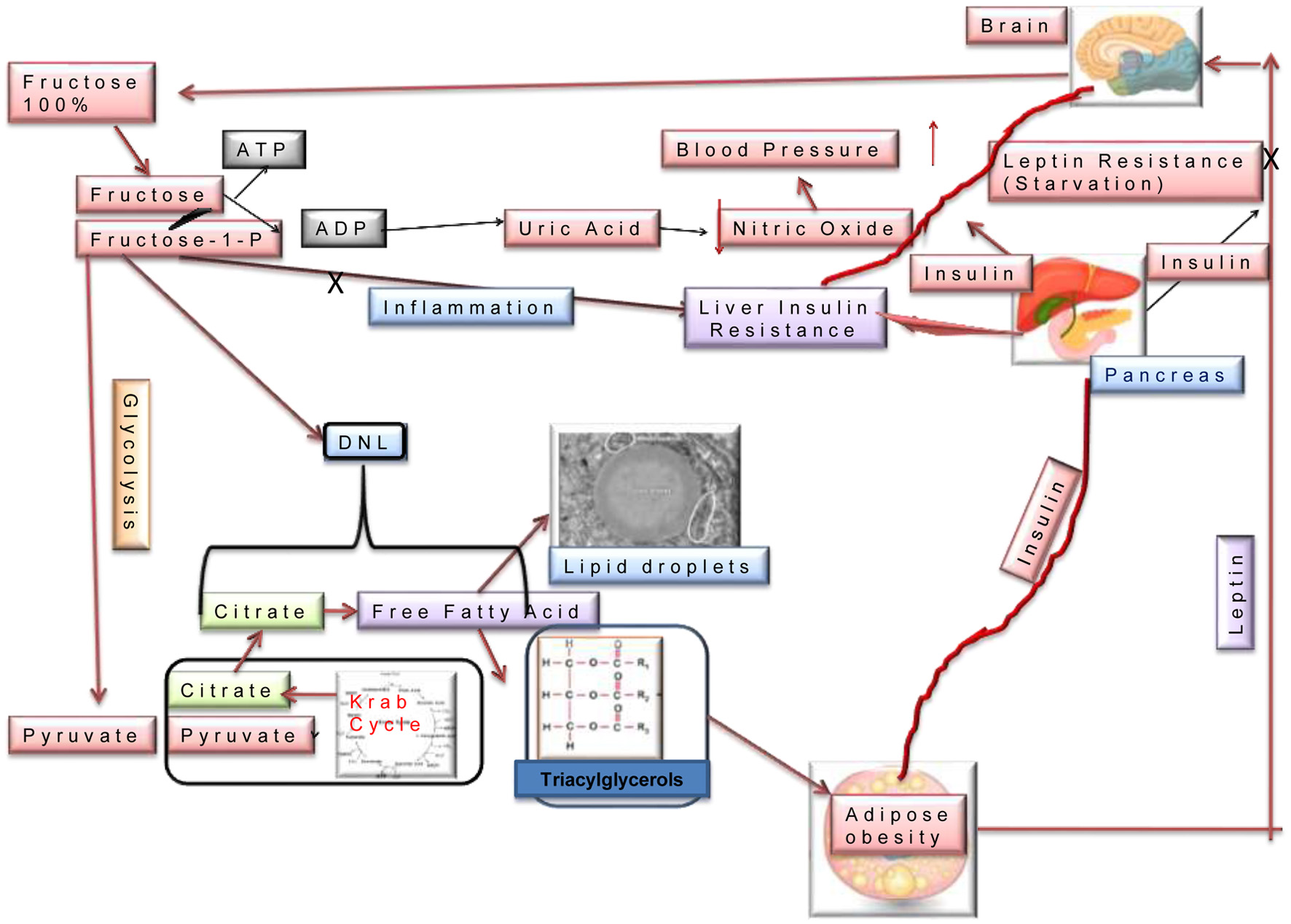 Click for large image | Figure 1. Molecular mechanism of dietary consumption and metabolic disorders. |
 Click to view | Table 1. Lipid Oriented Cardiometabolic disorders |
CVD tests include total cholesterol, cholesterol of low density, cholesterol of high density, cholesterol of high density, triacylglycerol, very-low-density lipoproteins (VLDL), vertical auto profile (VAP), and cardiac risk. As markers of myocardial injury, cardiac-specific proteins are significant, since myocardial cell death leads to intracellular protein release into the bloodstream. The most reliable and sensitive Acute myocardial infarction indicators are cardiac-specific troponins I and T, combined with high-sensitivity assays (van der Linden et al., 2018). In addition to aspirin and beta-blockers, doctors also prescribe angiotensin-converting enzyme inhibitors and statins (Ciliberti et al., 2021; Hoedemaker et al., 2018). In some cases, doctors recommend procedures like coronary artery bypass surgery, balloon angioplasty, and valve repair and replacement.
3.2. Triacylglycerol, cholesterol, blood pressure, and heart
Inflammation, oxidative stress, endothelial function, and insulin are not adequately studied to determine how Trans-fatty acids affect cardiovascular disease. According to Sellem et al., (2023), Tran’s fats negatively affect LDL and HDL cholesterol levels, Inflammation, oxidative stress, endothelial function, and insulin. It is important to note that, although there are two types of LDL, the lipid profile test measures them both at the same time. Low-fat diets and statins can be used to reduce large buoyant or type A-LDLs, which make up about 80% of circulating LDLs. A second LDL species, small dense or type B-LDL (20%), is highly significant in predicting heart attack risk. It has been shown that large buoyant LDL particles do not cause plaque buildup in arteries (Borén et al., 2020; Tada et al., 2018). While statins lower LDL-C levels, they do not reduce cardiovascular risks. This is due to metabolic dysfunction that is caused by insulin resistance, which statins do not address (Athyros et al., 2018; Su et al., 2021). As reported in several studies (Kim et al., 2022; Ravnskov et al., 2018), statins reduce LDL-C, but do not reduce heart attacks. In a study that has been done in order to examine the effects of lowering triacylglycerol on coronary events, the research has shown that lowering triacylglycerol reduces the risk of death, although the results are still being monitored (Marston et al., 2019). The optimal or target level of the standard lipid profile and treatment options is mentioned in Table 2.
 Click to view | Table 2. Standard Lipid Profile and Treatment options |
It is well known that food and heart disease have a complex relationship. By reducing inflammation and triacylglycerol, omega-3 fatty acids can decrease the risk of heart disease and plaque buildup (Mason et al., 2020). Furthermore, insulin increases smooth muscle proliferation in coronary arteries, making them more susceptible to clots (Wang et al., 2022). Sugar consumption determines a person’s heart attack risk regardless of calorie consumption or obesity. However, by eliminating sugar from the diet, atherogenic particles (small dense LDL particles) are reduced, triacylglycerol are decreased, and HDL is raised, reducing the risk of heart disease (Lusting, 2021). As a result of refined carbohydrate intake (i.e. fibreless foods), and in particular sugar consumption, small dense LDL increases (Akhavan et al., 2020). Tran’s fat consumption has been linked to a higher level of biomarkers associated with cardiovascular disease, including tumor necrosis factor (TNF), interleukin-6 (IL-6), and C-reactive protein (Hadj Ahmed et al., 2018). In the US, Denmark, and other countries, Tran’s fat content in food has been regulated by law. Tran’s Fatty Acids are not only known for boosting cholesterol synthesis levels, but they are also known for damaging dietary cholesterol, blood cholesterol, lipoproteins, and cardiovascular disease risk. Cholesterol does not appear to be related to heart disease (Carson et al., 2020; Soliman, 2018). Tsoupras et al. (2018) found that serum cholesterol is not the only cause of cardiovascular diseases; platelet activating factors (PAF) and inflammation-induced factors also play a role. In blood profiles, LDL-C and non-HDL-C≥160 mg/dl are associated with CVD mortality risk (Abdullah et al., 2018). It is unclear how weight loss and weight regain affect cardiometabolic outcomes in a biochemical manner. According to the study, decreased circulating phosphatidylcholines (PCs) and sphingomyelins (SMs) may reduce cardiovascular risk by impacting Total Cholesterol and LDL-C during weight loss and maintenance (Papandreou et al 2021b). A study has been conducted specifically to examine the relation between circulating metabolites and the changes in adiposity caused by diet-induced weight loss. Additionally, the study examined changes in these metabolites following weight loss maintenance in relation to body weight and adiposity regain. Citric acid and lipid species have been observed to change with weight loss. As a result of these changes, weight and adiposity regain is associated with adipose lipid metabolism (Papandreou et al., 2021a).
Among the several important parameters, triacylglycerol are much more significant than LDL. The HR ratio between triacylglycerol and heart disease is 1.8 (80% higher risk of heart attack) in comparison to LDL at 1.3. Triacylglycerol are the better biomarkers in terms of heart disease than LDL (Malhotra, 2021). The triacylglycerol level has consistently been associated with heart disease, stroke, and heart attacks, especially in patients with diabetes and low HDL levels. It has been documented that elevated triacylglycerol levels are detrimental to the liver and pancreas. However, there are contradictory results regarding the risk of heart disease associated with high triacylglycerol levels (Shemesh and Zafrir, 2019). Polyunsaturated fatty acids (PUFAs) and monounsaturated fatty acids (MUFAs) were associated with lower CVD risk, while saturated fatty acids and Trans fat intakes were associated with a higher CVD risk. SFAs were inversely associated with CVD when replaced with MUFAs and PUFAs (Guasch-Ferré et al., 2019; Sellem et al., 2023). Many experts do not believe that triacylglycerol cause heart problems. CVD risk is increasingly linked to postprandial triacylglycerol (ppTG), which rise after meals. Sugars did not seem to have an overall significant effect on ppTG response, but sensitivity analysis revealed fructose had a significant effect on ppTG response. There is evidence that fructose reduces lipoprotein lipase activity in adipose tissue, which is associated with less insulin secretion stimulated by fructose than by glucose. Further, fructose consumption is linked to increased de novo lipogenesis in the liver, leading to increased very low density lipoproteins and triacylglycerol (VLDL-TGs). Lee et al., 2020, reported that fructose increases ppTG more rapidly than glucose because it prefers lipogenesis to glucose. According to Peoples et al., (2019), chronic diseases and mitochondrial dysfunction are interconnected (Figure. 2).
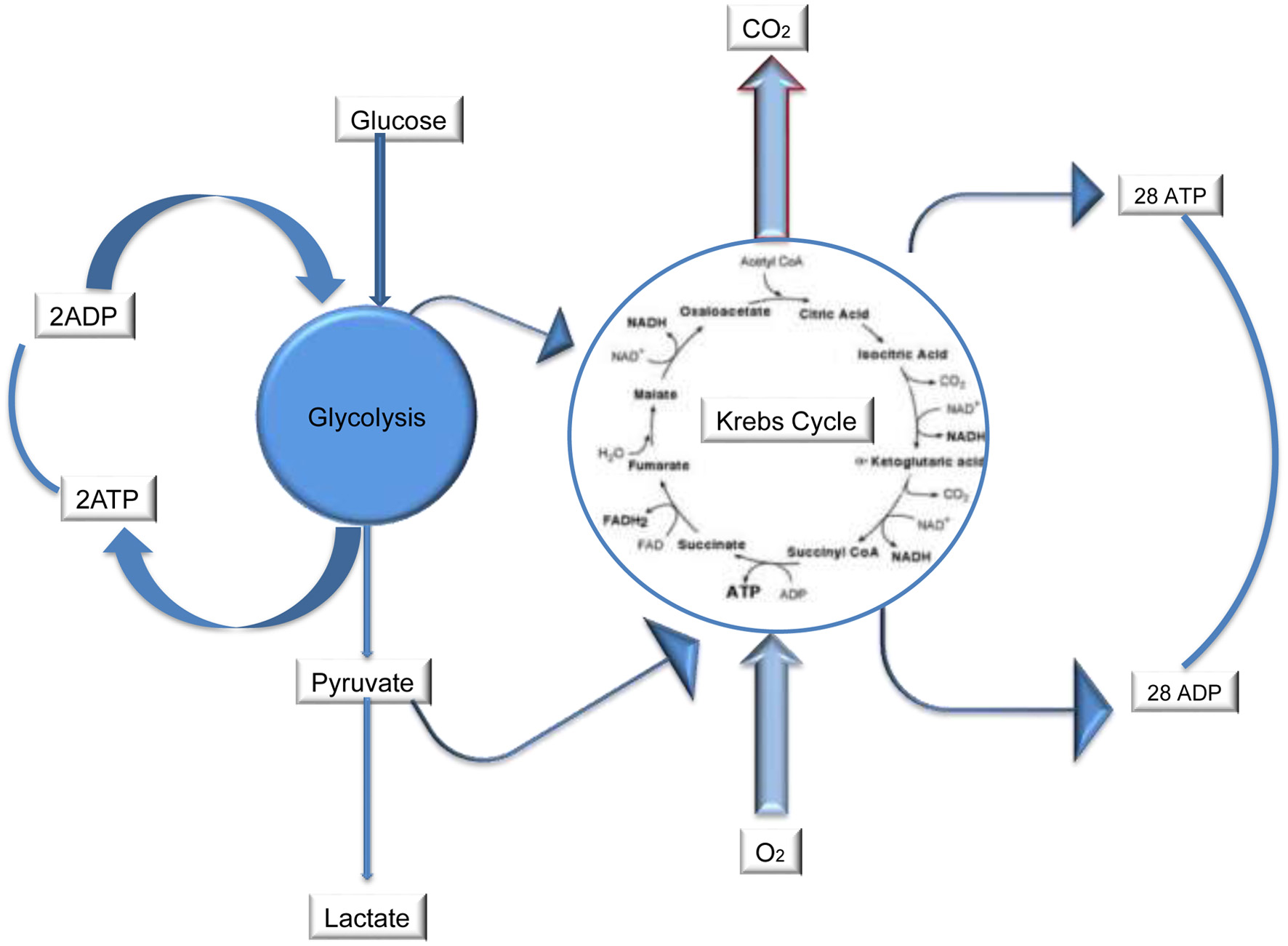 Click for large image | Figure 2. Mitochondria dysfunction and Cardiovascular Diseases (CVDs). |
It is estimated that mitochondria occupy about 30% of the total cell volume and produce 30 kg of ATP per day in cardiomyocytes (Lin et al., 2019). A cell’s mitochondria have their own genetic code and DNA separate from the nucleus’s DNA. Exercise is the most efficient means of generating mitochondria (Braga et al., 2021). It is important to maintain optimal blood glucose and oxygen levels, as well as mitochondrial capacity (Ashleigh et al., 2023; Flockhart et al., 2021). An increase in glucose entering the cell causes glycation and oxidative stress (Ayinde et al., 2020; Nellaiappan et al., 2019; Zhang et al., 2020) via phosphoinositide 3-kinase, Adenosine monophosphate-activated protein kinase, mammalian target of rapamycin (PI3K+, AMPK+, mTOR+). As glucose is burnt by mitochondria, an AMP-kinase partially inhibits mTOR, autophagy occurs but not entirely, and some dead cells are eliminated. Over time, this may lead to heart disease (Buemann and Uvnäs-Moberg, 2020). Diet modulates each of these checkpoints, including circulation of serum triacylglycerol and the clearance of LDL particles from adipose tissue (Lusting, 2021). For this reason, TG/HDL ratios (high-density lipoproteins) are the most accurate biomarkers for heart diseases. Another significant parameter is HDL, which indicates good cardiovascular health if it is above 60. If HDL is lower than 40, heart disease risk is higher (Kosmas et al., 2023). Despite the lack of a clear link between high-density lipoprotein cholesterol and cardiovascular disease, it has been hypothesized that HDLs atheroprotective function rests on its biological activity rather than its cholesterol content. The relationship between HDL functional characteristics and acute coronary syndrome, however, has not been extensively explored. This case-control study is nestled within a randomized trial involving participants who followed low-fat or Mediterranean diets in PREDIMED. An acute coronary syndrome case (N = 167) was matched (1:2) with a control patient by gender, age, intervention group, body mass index, and follow-up time. An increased risk of acute coronary syndrome and its manifestations in individuals at high cardiovascular risk has been associated with low cholesterol efflux capacity values, pro-oxidant/proinflammatory HDL particles, and sphingosine-1-phosphate and apolipoprotein A-I levels of HDL particles (Soria-Florido et al., 2020). Inflammation and cardiovascular risk are related to cell membrane fatty acid composition. A Mediterranean population at high risk of heart disease is found to have interrelationships between inflammation indicators and both blood cell membrane fatty acid composition and HDL structure/function parameters (Muralidharan et al., 2022). Healthy hearts are tested for cholesterol, HDL, TG, homocysteine levels, alanine aminotransferases (ALT), aspartate aminotransferases (AST), uric acid, fasting insulin, fasting glucose, and hemoglobin A1c. Serum homocysteine (Hcy) levels are an indication of your diet and epigenetic when patients have a family history of heart disease (Azzini et al., 2020). As an amino acid associated with heart disease, hydroxycitrate (Hcy) should be removed from the bloodstream and eliminated. Unless this is done, it will accumulate in blood vessels, causing inflammation and heart disease. This amino acid must be removed from the bloodstream and eliminated. Folic acid can help remove Hcy from the body if the level of Hcy is high. High Hcy contributes to a high risk for heart disease. Despite the fact that many factors contribute to blood pressure variation, there is still little information about how it occurs. Obesity and hyperlipidemia are associated with elevated blood pressure variability (Eghbali et al., 2018). Cardiovascular mortality and morbidity are predicted by a change in blood pressure and heart rate every 30 minutes (Schroeder et al., 2019). There is no simple method to test mitochondria (Li et al., 2020; Jacob et al., 2021). If you have healthy, functioning mitochondria, it doesn’t matter what you weigh. If you have dull, dilapidated, and under decay, it doesn’t matter. Those with a large waist circumference often have metabolic problems, and they will need to change their diet to raise insulin levels (Valenzuela et al., 2023). A low waist circumference and high blood pressure may indicate salt rather than sugar as the cause. A high waist circumference and abnormal blood pressure may indicate a salt or stress issue (Lusting, 2021). Diabetes patients may develop cardiovascular complications as a result of metabolic syndrome, which is extremely common. Therefore, those caring for diabetic patients must be aware of whether they also meet the MetS criteria. A simple clinical approach to identifying individuals for intervention can serve as an effective tool to reduce CVD and type 2 diabetes (Arnett et al., 2019). An individual’s dietary interventions should be based on their family history, anthropometric measurements, and metabolic profile. No large-scale high-resolution studies have been conducted to determine whether certain diets affect cardiovascular disease risk, including low-carbohydrate, low-fat, Paleolithic diet, ketogenic, Vegetarian, Mediterranean, and low-salt diets. A poor metabolic response to a particular meal is associated with low postprandial triacylglycerol and glucose levels (Berry et al., 2020).
3.3. Diet and dietary habits
A key component of cardiovascular treatment is diet management. There is nothing more nutritious than real food with color. This is because plants contain antioxidants that humans cannot produce (Pérez-Torres et al., 2021). It has been shown that vegetarian diets, as well as the Mediterranean diet, have a significant impact on gut microbiome and cardiovascular disease risk (Tindall et al., 2018; Wang et al., 2021). Spain, Greece, Italy, and other countries near the Mediterranean Sea follow the Mediterranean diet. They mainly consume fresh fruit, vegetables, grains, nuts, and olive oils. The Mediterranean diet has been shown to reduce cholesterol, reduce oxidative stress, inflammation, platelet aggregation, and modify hormones and growth factors that are involved in cancer. In addition to inhibiting nutrient-sensing pathways, specific amino acids are reduced in the gut microbiota, which is responsible for producing metabolites that affect metabolic health (Tosti et al., 2018; Gantenbein and Kanaka-Gantenbein, 2021). The MedDiet is one of the best dietary patterns analyzed in relation to CVD risk and other health outcomes in a meta-analysis that summarized and discussed the evidence from epidemiological and clinical trials analyzing its impact on CVD risk (Salas-Salvadó et al., 2018). It is well established that postprandial glycemic and insulinemic responses are affected by the quality of carbohydrates consumed, whether measured by glycemic index, glycemic load, or carbohydrate quality index. It is unclear, however, whether plasma metabolites involved in different biological pathways could be used to study carbohydrate quality indices functionally. It was found that the glycemic index (GI), the glycemic load (GL), and the carbohydrate quality index (CQI) were linked to the metabolite of a Mediterranean population at high cardiovascular disease risk (Bulló et al., 2021).
Paleo diets are among the most popular dietary patterns, as they are based on wild foods consumed during the Paleolithic period. According to studies, the Paleo diet can reduce the risk of several health outcomes, including metabolic syndrome, diabetes, overweight or obesity, and cardiovascular diseases (de la O et al., 2021). Patients with diabetes type 2 lose weight rapidly and sensitively on the ketogenic diet, and their hemoglobin A1c levels fall, which is associated with favorable changes in biomarkers. It is also known to cause a significant increase in the levels of low-density lipoprotein cholesterol (O’Neill and Raggi, 2020), so many physicians do not endorse it. During 56 weeks, ketogenic diet use for obese subjects with cholesterol levels above 6 mmol/L was compared to normal cholesterolemia subjects. The data showed significant reductions in body mass index and body weight in both groups (P < 0.0001). Total cholesterol, LDL cholesterol, triacylglycerol, and blood glucose levels all decreased significantly (P > 0.0001) after the treatment, but HDL cholesterol increased significantly (P > 0.0001). In this study, Dashti et al. (2006) demonstrated that patients with high total cholesterol and obese subjects that follow low carbohydrate diets can continue to do so for longer periods of time. There was evidence that vegan diets were associated with a lower BMI, a lower total cholesterol level, a lower glucose level, a lower level of inflammation, and a lower blood pressure level in studies that looked at vegan diets (Kaiser et al., 2021). It was examined whether vegan diets were adequate for European populations in terms of macronutrients and micronutrients. Vegan diets are lower in protein as compared to conventional diets. Furthermore, veganism is associated with lower intakes of vitamins B2, Niacin (B3), B12, D, iodine, zinc, calcium, potassium, and selenium. As a result of their low B12 intake (0.024–0.49 μg, 2.4 μg recommended), vegetarians have low calcium intake (750 mg/day). It has a moderate glycemic load and does not cause deficiencies in vitamins A, B1, B6, C, E, iron, phosphorus, magnesium, copper, or folate. A vegan diet may cause deficiencies in several micronutrients (vitamin B12, zinc, calcium, and selenium). There is no conclusive evidence that inadequate micro- and macronutrient intakes cause health impairments (Bakaloudi et al., 2021). The Mediterranean diet is one example of a dietary pattern that can modulate exosome-transported lncRNAs and miRNAs through exosome RNA modulation. A study provides the first evidence that lncRNAs and miRNAs may be viable targets for nutritional interventions, although their validation in a larger cohort is necessary (Mantilla-Escalante et al., 2021). There is evidence from both observational studies and randomized controlled trials that this diet benefits markers of cardiovascular disease, including waist-to-hip ratio, lipid levels, and inflammation markers, as well as primary outcomes like death (Zhou et al., 2023). There is no doubt that these improvements are comparable to those of well-established tools that prevent cardiovascular diseases, such as aspirin, beta-blockers, angiotensin-converting enzyme inhibitors, and exercise (Rosato et al., 2019; Pocovi-Gerardino et al., 2021; Lutski et al., 2022). In a study conducted by Morel et al., 2020, lipopolysaccharide-binding protein was associated with metabolic endotoxemia, inflammation, and cardiometabolic outcomes. Using a multi-omics integrative approach, the effect of the Med Diet versus nuts supplementation on circulating metabolites and their relationship with cardiometabolic health was evaluated. In addition, a multi-omics integrative study examined whether changes in gut microbiota composition were associated with changes in metabolomic profiles. Specifically, 65 circulating metabolites decreased with the Med Diet, including lipids, acylcarnitines, amino acids, steroids and TCA intermediates. Additionally, glucose, insulin, and HOMA-IR decreased as well. Based on the network analysis, two main clusters of genera were identified, including PC species, ChoE (20:5), TGs and medium/long-chain acylcarnitines (Galié et al., 2021). It has been reported that phytochemicals are responsible for regulating the lipid metabolic interventions that are responsible for cholesterol biosynthesis, absorption, transport, and elimination (Centner et al., 2023; Islam et al., 2021; Buscemi et al., 2021). This study has compared various dietary patterns and their cardiometabolic relations (Table 3). By changing your diet and eating habits, you can more effectively reverse metabolic syndrome without side effects (Figure 3).
 Click to view | Table 3. Comparison of different dietary parameters for healthy cardiometabolic system |
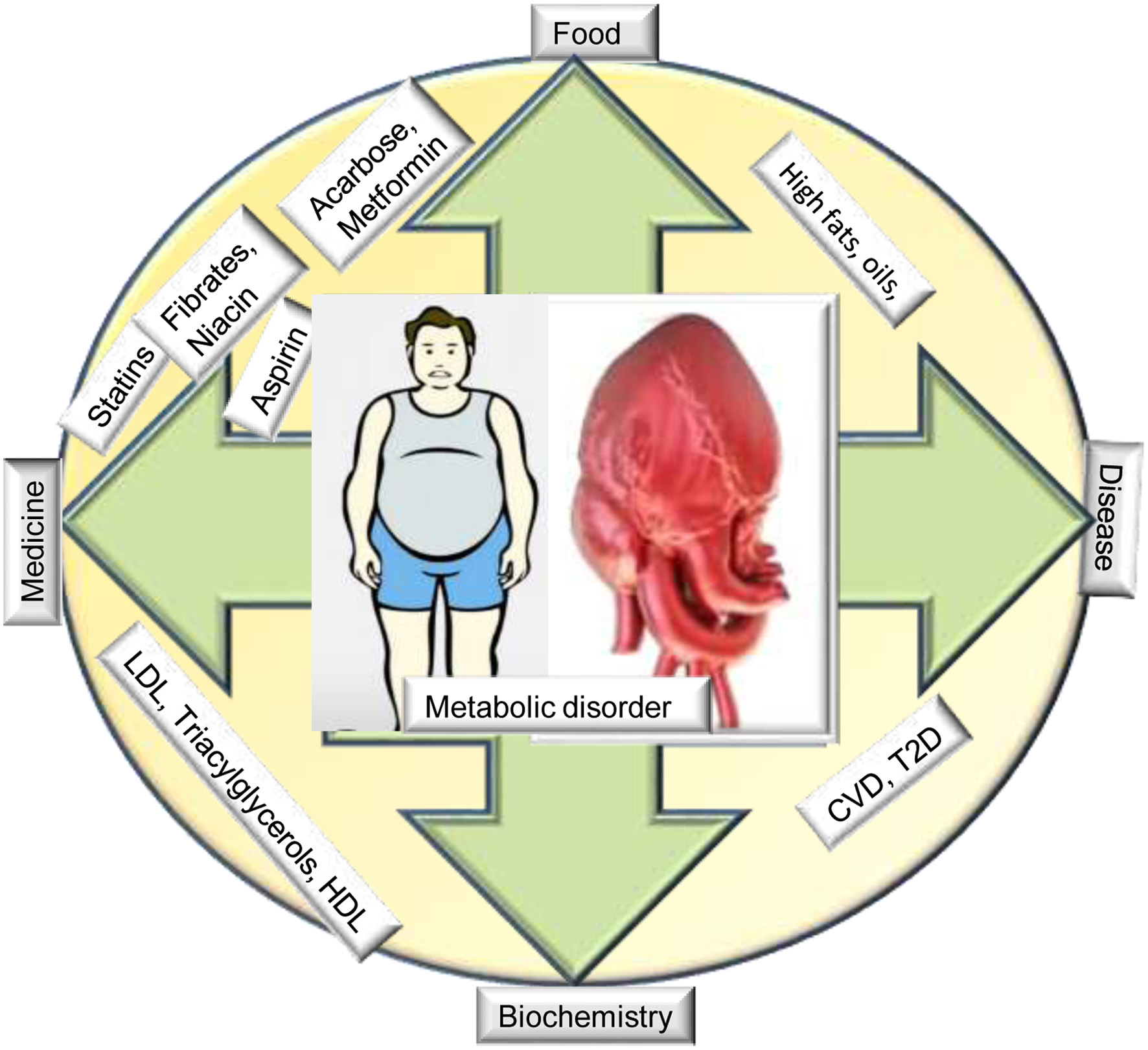 Click for large image | Figure 3. Relationship between food, metabolic disorder and medicine. |
Most of our medicines treat symptoms related to mitochondrial perturbations, like blood pressure, but not mitochondria (Zujko et al., 2021). High TG levels can only be treated by diet (Dong et al., 2020; Rodríguez-Correa et al., 2020). Individuals respond differently to different diets, and others do not benefit at all. In spite of dietary recommendations, many people consume insufficient amounts of dietary fiber or consume inappropriate fiber, which is known to cause type 2 diabetes mellitus. It has been shown that medical nutrition therapy (MNT) can be a useful tool for preventing and managing type 2 diabetes mellitus (T2DM). In addition to improving blood sugar control and reducing sugar spikes, fiber-rich diabetes nutrition reduces hyperinsulinemia and helps patients manage their weight (Salvia and Quatromoni, 2023). A fiber-rich diet is essential for diabetics and patients with associated conditions. Fiber intake should be increased through diet or supplementation (Saboo et al., 2022). There has been no comparison between vegan and ketogenic diets in terms of biomarkers or events. In ketogenic diets, there are fewer carbs (10%), more fat (70%), and more protein (20%), which is mainly made up of butter eggs, cream, bacon, and green vegetables (Steck and Murphy, 2020). The consumption of pulses regularly as part of an adlibitum diet has been shown to be beneficial in several studies. Since pulses are low in calories, they can be included in diets to manage metabolic syndrome risk factors (Said et al., 2022). Vegans and vegetarians have lower BMIs than non-vegetarians. According to WHO 2021, everyone should consume at least 400 grams of fruits and vegetables (excluding potatoes and starchy tubers) a day for a healthy cardiovascular system (WHO, 2021).
| 4. Conclusion | ▴Top |
A proper diet and lifestyle can help control cholesterol and triacylglycerol, which are primarily responsible for cardiovascular disease. Cardiovascular disease is primarily caused by metabolic disorders. Coronary heart disease is strongly linked to mitochondrial dysfunction. Geographic and cultural factors influence diet patterns. Exercise, healthy eating habits, and nutrition can reduce the risk of cardiovascular disease. There is a need to understand the molecular and cellular mechanism behind CVD and develop targeted therapies. The vegetarian Mediterranean diet has better cardiovascular health effects than other popular diets, such as ketogenic and the Paleo diet. A healthy lifestyle and conventional medications are needed in order to treat high lipid levels of patients. Nutritional interventional studies are more complicated than single drugs used in clinical trials. Genetic, inflammatory, nutritional, and immune factors all contributed to cardiometabolic syndrome pathogenesis. Studies on genetic and inflammatory markers, along with nutritional factors, and immune responses, will help us better understand it.
Acknowledgments
I would like to acknowledge Prof. Jawar Singh from IIT Patna for his technical assistance.
The authors did not receive support from any organization for the submitted work. The authors have no relevant financial or non-financial interests to disclose.
Conflict of interest
The author declares that they have no competing interests
| References | ▴Top |